Trauma and post-traumatic stress disorder (PTSD) are complex phenomena with profound effects on the brain. Understanding the neurobiological underpinnings of trauma and PTSD is crucial for developing effective treatments and interventions. In this extensive exploration, we’ll delve deep into how trauma impacts the brain, the neural mechanisms underlying PTSD, and the implications for treatment and recovery.
Introduction
Trauma is an experience that overwhelms an individual’s capacity to cope, often resulting in a range of psychological and physiological responses. While trauma can take many forms, including physical abuse, natural disasters, combat exposure, and interpersonal violence, the effects on the brain can be strikingly similar across different types of trauma.
Post-traumatic stress disorder (PTSD) is a psychiatric condition that can develop in individuals who have experienced or witnessed a traumatic event. It is characterized by symptoms such as intrusive memories, hyperarousal, avoidance behavior, and negative alterations in mood and cognition. PTSD can have a profound impact on various aspects of an individual’s life, including their relationships, work, and overall quality of life.
Neurobiology of Trauma
To understand how trauma impacts the brain, it’s essential to examine the neural circuits and structures involved in the stress response. The brain’s response to stress is orchestrated by a complex interplay of neurotransmitters, hormones, and neural circuits, collectively known as the stress response system.
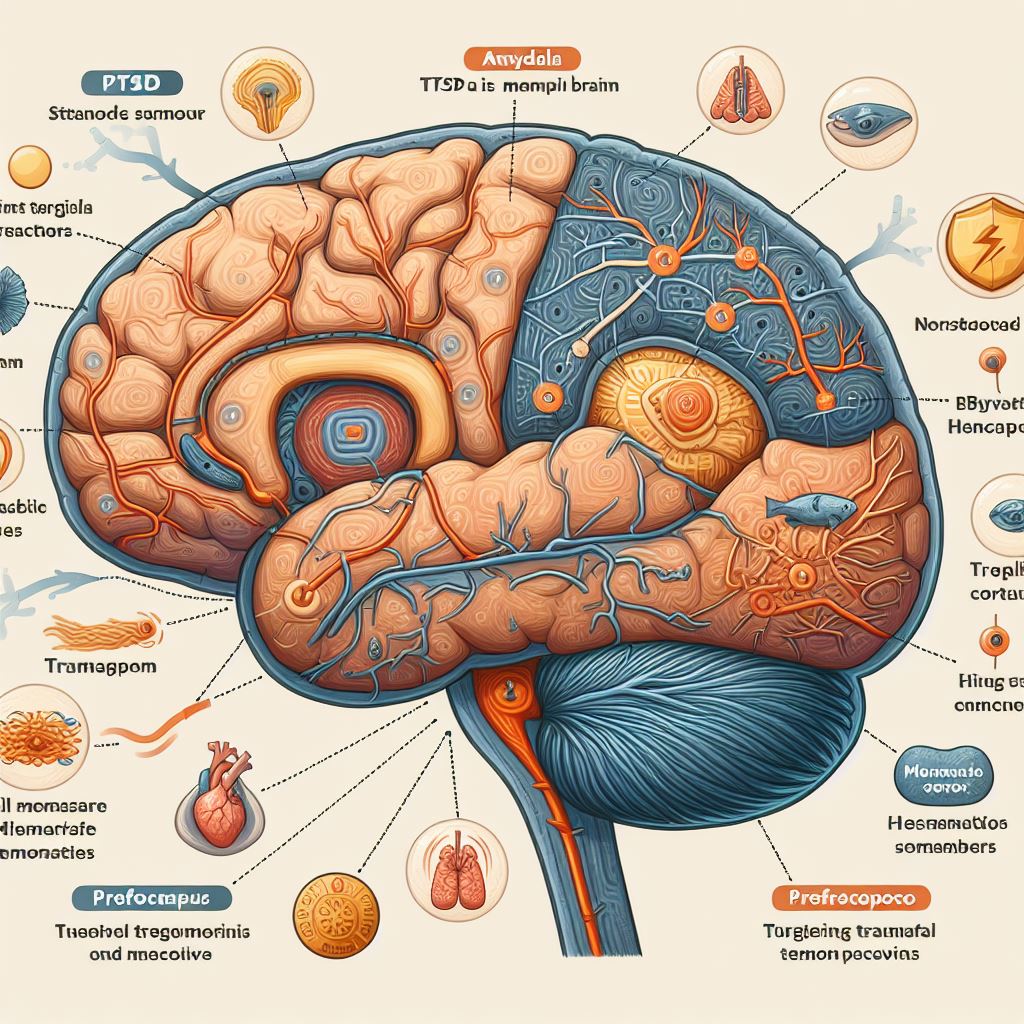
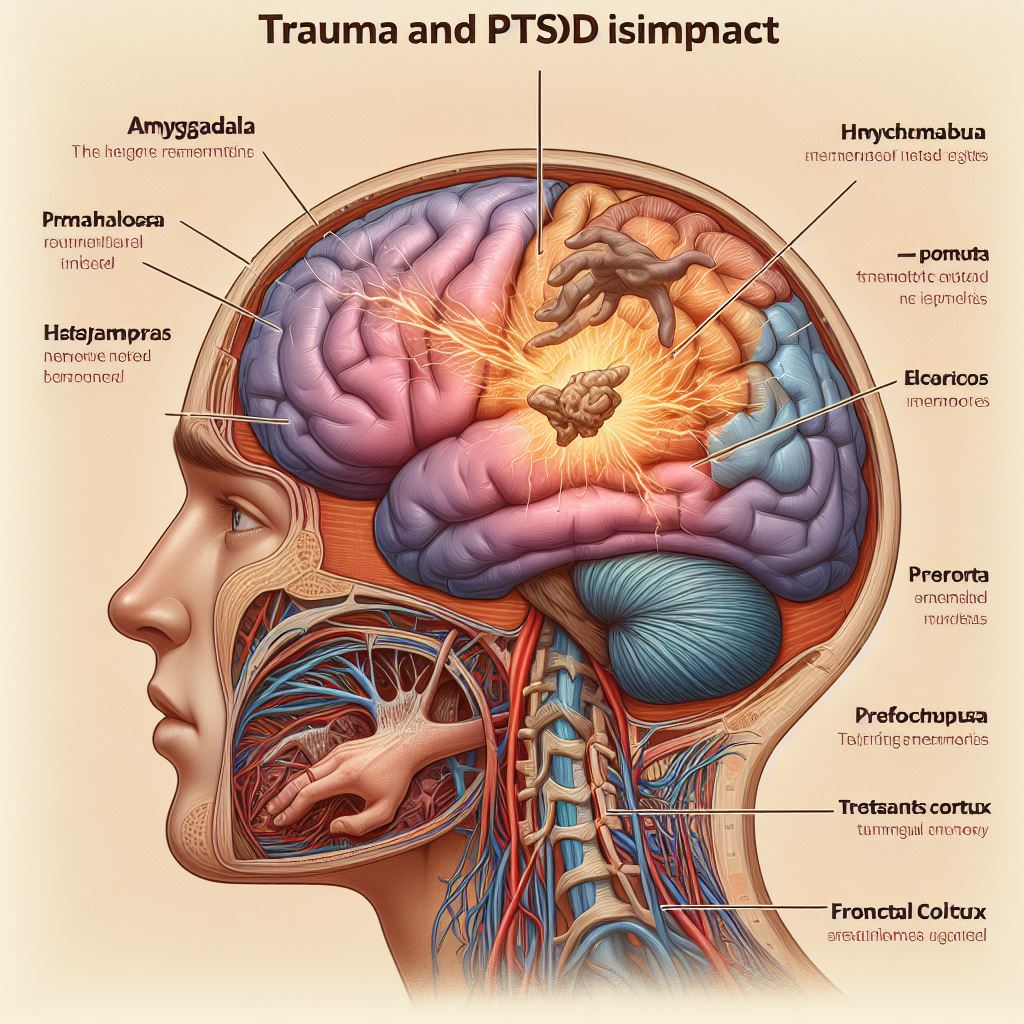
- Amygdala: The amygdala, an almond-shaped structure located deep within the brain’s temporal lobes, plays a central role in processing emotions, particularly fear and threat detection. When faced with a perceived threat, sensory information is rapidly transmitted to the amygdala, triggering a cascade of physiological and behavioral responses. In individuals with PTSD, the amygdala is often hyperactive, leading to heightened fear responses and exaggerated emotional reactions to trauma-related stimuli.
- Hippocampus: The hippocampus, a seahorse-shaped structure located in the medial temporal lobe, is critical for memory formation and retrieval. Chronic stress and trauma can lead to structural and functional changes in the hippocampus, including shrinkage and impaired neurogenesis. As a result, individuals with PTSD may experience difficulties in encoding, consolidating, and retrieving memories, particularly those related to the traumatic event.
- Prefrontal Cortex (PFC): The prefrontal cortex, particularly the ventromedial prefrontal cortex (vmPFC) and dorsolateral prefrontal cortex (dlPFC), plays a key role in executive functions such as decision-making, impulse control, and emotion regulation. Trauma can disrupt the functioning of the PFC, leading to deficits in cognitive flexibility, emotion regulation, and inhibitory control. Dysfunction in the PFC may contribute to symptoms of impulsivity, emotional dysregulation, and difficulty in engaging in adaptive coping strategies.
- Hypothalamic-Pituitary-Adrenal (HPA) Axis: The stress response is coordinated by the hypothalamic-pituitary-adrenal (HPA) axis, a complex neuroendocrine system involving the hypothalamus, pituitary gland, and adrenal glands. In response to stress, the hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH). ACTH then signals the adrenal glands to release cortisol, the body’s primary stress hormone.
Trauma and chronic stress can dysregulate the HPA axis, leading to alterations in cortisol secretion and sensitivity. In individuals with PTSD, cortisol levels may be dysregulated, with some studies reporting blunted cortisol responses to stressors, while others demonstrate heightened basal cortisol levels. These alterations in cortisol function can have widespread effects on the brain, including impairments in memory, learning, and emotional regulation.
- Neurotransmitters: Trauma can disrupt the balance of neurotransmitters in the brain, including serotonin, dopamine, and norepinephrine. These neurotransmitters play crucial roles in mood regulation, arousal, and stress response. Dysregulation of neurotransmitter systems has been implicated in the pathophysiology of PTSD, contributing to symptoms such as depression, anxiety, and hypervigilance. Medications that target neurotransmitter systems, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), are commonly used in the treatment of PTSD to modulate neurotransmitter function and alleviate symptoms.
- Neuroplasticity: The brain exhibits remarkable plasticity, or the ability to reorganize its structure and function in response to experiences. While trauma can lead to maladaptive changes in the brain, such as alterations in amygdala and hippocampal volume, it’s also possible for the brain to undergo positive changes through interventions such as therapy, mindfulness practices, and pharmacological treatments. These interventions can promote neuroplasticity, fostering resilience and facilitating recovery from trauma-related symptoms.
Neural Mechanisms of PTSD
PTSD is associated with a range of neurobiological abnormalities, reflecting the complex interplay of genetic, environmental, and psychological factors underlying the disorder. While the precise mechanisms remain incompletely understood, several key neural circuits and processes have been implicated in the pathophysiology of PTSD.
- Fear Circuitry: PTSD is characterized by alterations in the brain’s fear circuitry, which includes the amygdala, hippocampus, and prefrontal cortex. Functional neuroimaging studies have consistently demonstrated hyperactivity of the amygdala and hypoactivity of the vmPFC in individuals with PTSD, suggesting an imbalance between the threat detection system and the regulatory mechanisms that govern fear responses. This dysregulation in fear circuitry may contribute to symptoms such as hypervigilance, exaggerated startle responses, and intrusive memories of the traumatic event.
- Hippocampal Dysfunction: Structural and functional abnormalities in the hippocampus are commonly observed in individuals with PTSD. Reduced hippocampal volume has been consistently reported in neuroimaging studies of PTSD, and this shrinkage is thought to reflect the detrimental effects of chronic stress on hippocampal neurons, including decreased dendritic branching, synaptic loss, and impaired neurogenesis. Hippocampal dysfunction may contribute to deficits in explicit memory processing and contextual modulation of fear responses, as well as the fragmentation and intrusiveness of traumatic memories.
- Prefrontal Cortex Dysfunction: Dysfunction in the prefrontal cortex, particularly the vmPFC and dlPFC, is implicated in the pathophysiology of PTSD. Reduced activation of the vmPFC during emotional regulation tasks and deficits in cognitive control mediated by the dlPFC have been reported in individuals with PTSD. These abnormalities in prefrontal cortex function may underlie difficulties in emotion regulation, inhibitory control, and cognitive flexibility observed in PTSD, as well as impairments in the extinction of conditioned fear responses.
- Altered Resting-State Connectivity: Resting-state functional connectivity refers to the temporal correlation of spontaneous neural activity between different brain regions in the absence of task demands. Alterations in resting-state connectivity have been observed in individuals with PTSD, with studies reporting disrupted connectivity within the default mode network (DMN), salience network, and central executive network. These changes in connectivity patterns may reflect aberrant information processing, attentional biases, and alterations in self-referential processing observed in PTSD.
- Epigenetic Modifications: Emerging evidence suggests that trauma exposure can lead