Trauma can have a profound impact on addiction, influencing both the development and progression of substance use disorders. The relationship between trauma and addiction is complex and multifaceted:
- Self-Medication: Many individuals who have experienced trauma turn to substances as a way to self-medicate. They may use drugs or alcohol to numb emotional pain, cope with anxiety, depression, or post-traumatic stress disorder (PTSD), or to temporarily escape their reality.
- Self-medication is a significant concept in understanding the relationship between trauma and addiction. Individuals who have experienced trauma often turn to substance use as a means to cope with or alleviate the distressing symptoms and emotional pain associated with their traumatic experiences. Here are key aspects of self-medication in the context of trauma’s impact on addiction:
- Coping Mechanism for Trauma Symptoms: People who have experienced trauma, especially those with unresolved or untreated trauma, may use drugs or alcohol to numb intense emotions, suppress disturbing memories, or manage symptoms of post-traumatic stress disorder (PTSD), such as anxiety, depression, or insomnia.
- Temporary Relief: Substance use can provide temporary relief or a sense of escape from the psychological pain caused by trauma. However, this relief is short-lived and can lead to a cycle of increased use as the effects of the substance wear off.
- Negative Reinforcement: The temporary alleviation of trauma-related distress through substance use reinforces the behavior, creating a pattern where the individual increasingly relies on substances to cope with their symptoms.
- Increased Vulnerability to Addiction: The use of substances as a coping mechanism for trauma can increase the risk of developing an addiction. The brain’s reward system can become linked to substance use as a way to escape trauma-related distress.
- Worsening of Trauma Symptoms: Over time, substance use can exacerbate the underlying trauma symptoms. It can lead to increased anxiety, paranoia, depression, and in some cases, can trigger flashbacks or worsen PTSD symptoms.
- Avoidance of Treatment: Engaging in self-medication can delay or prevent individuals from seeking appropriate treatment for their trauma, leading to a prolonged cycle of trauma and addiction.
- Impaired Emotional Processing: Substance use can impair the ability to process and work through traumatic experiences. It often serves as a barrier to emotional healing and resolution of trauma.
- Physical Health Consequences: Besides the psychological aspects, self-medication with substances can lead to significant physical health issues, including those related to the substance itself and the neglect of general health and wellbeing.
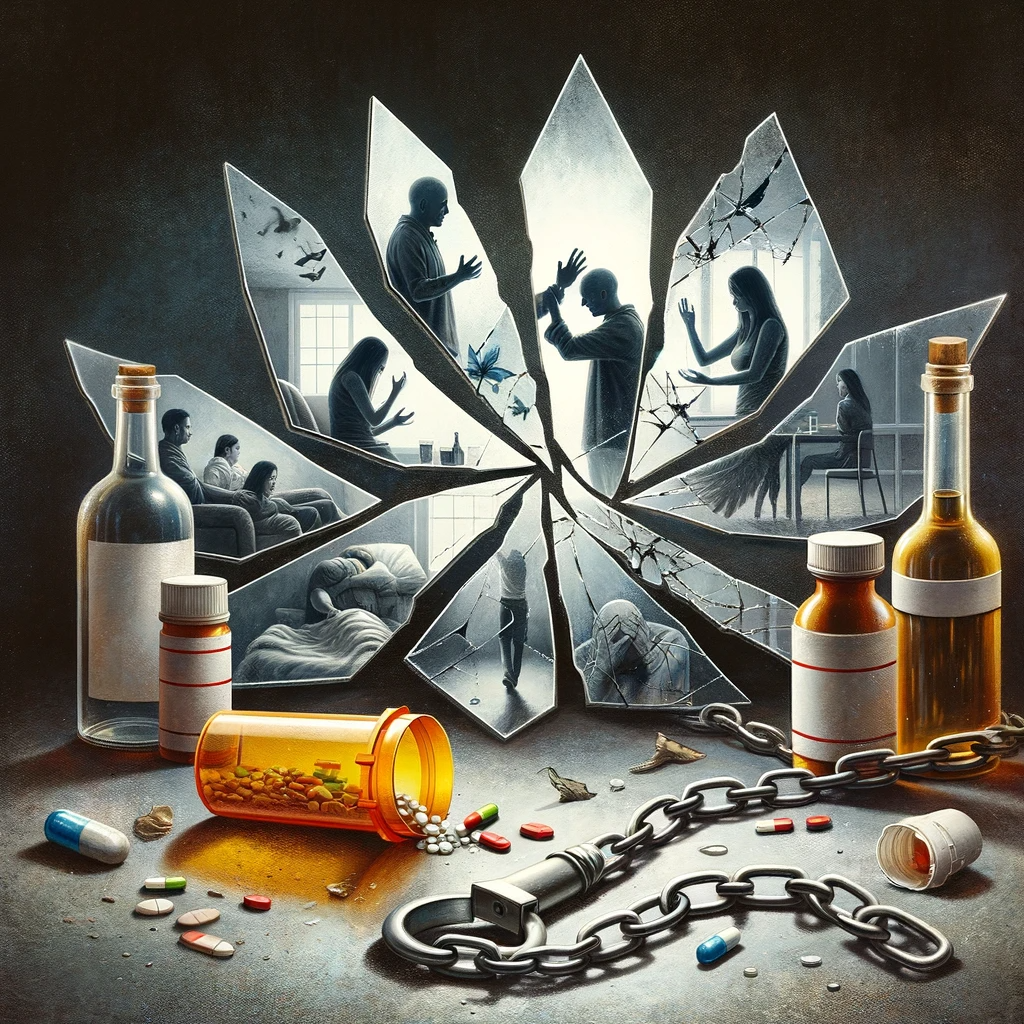
- Relationships and Social Functioning: The use of substances as a coping mechanism can strain personal and professional relationships and impair social functioning, further isolating the individual and exacerbating the impact of the trauma.
- Need for Integrated Treatment Approach: Addressing self-medication in the context of trauma requires an integrated treatment approach that simultaneously addresses the substance use disorder and the underlying trauma.
- Understanding self-medication is crucial in the treatment of individuals with trauma-related addiction. It highlights the need for comprehensive care that includes trauma-informed approaches, psychological support, and therapies specifically tailored to address both the trauma and the addiction.
- Self-medication is a significant concept in understanding the relationship between trauma and addiction. Individuals who have experienced trauma often turn to substance use as a means to cope with or alleviate the distressing symptoms and emotional pain associated with their traumatic experiences. Here are key aspects of self-medication in the context of trauma’s impact on addiction:
- Vulnerability to Addiction: Trauma, especially in early life such as childhood abuse or neglect, can increase vulnerability to addiction. Trauma can alter brain chemistry and stress responses, making individuals more susceptible to substance use disorders.
- The connection between trauma and increased vulnerability to addiction is a critical aspect of understanding substance abuse disorders. Trauma, particularly unresolved or chronic trauma, can significantly heighten an individual’s risk of developing addiction. This vulnerability manifests through various mechanisms:
- Altered Brain Chemistry: Traumatic experiences can alter brain chemistry, particularly in areas related to stress, emotion regulation, and reward. These changes can increase susceptibility to the addictive properties of substances, as they may temporarily alleviate trauma-related distress.
- Coping Mechanism: Individuals who have experienced trauma often struggle with intense emotions and painful memories. Substances can become a coping mechanism, providing temporary relief or a means of escape from these feelings.
- Self-Medication: As with coping, the concept of self-medication is prevalent. Trauma survivors may use drugs or alcohol to manage symptoms of PTSD, anxiety, depression, or insomnia, which are common after traumatic experiences.
- Increased Sensitivity to Stress: Trauma can heighten an individual’s response to stress. Substances that soothe or numb stress responses can become particularly appealing, leading to dependency as a way to manage daily stressors.
- Impaired Judgment and Impulsivity: Trauma, especially during developmental years, can impact decision-making and impulse control. This impairment can lead to risky behaviors, including substance experimentation and abuse.
- Social and Relationship Issues: Traumatic experiences often lead to difficulties in social interactions and relationships. Substance use might initially seem like a way to ease social anxiety, enhance socialization, or cope with relationship problems.
- Avoidance Behaviors: Avoidance of trauma-related thoughts and emotions is a common response. Drugs or alcohol can be used as tools to avoid facing or processing traumatic memories, perpetuating a cycle of avoidance and substance use.
- Lowered Self-Esteem: Trauma can severely impact self-esteem and self-worth, making individuals more susceptible to substance use as a means of coping with feelings of worthlessness or hopelessness.
- Development of Co-occurring Disorders: Trauma survivors are at higher risk for mental health disorders, which can co-occur with substance use disorders. This dual diagnosis requires integrated treatment approaches.
- Generational Patterns: In some cases, trauma and substance use disorders can be intergenerational. Children exposed to trauma or familial substance abuse are at a higher risk of developing similar patterns.
- Understanding the link between trauma and vulnerability to addiction highlights the importance of addressing trauma in substance abuse treatment. It underscores the need for trauma-informed care approaches that recognize and treat the underlying trauma as a core component of recovery from addiction.
- The connection between trauma and increased vulnerability to addiction is a critical aspect of understanding substance abuse disorders. Trauma, particularly unresolved or chronic trauma, can significantly heighten an individual’s risk of developing addiction. This vulnerability manifests through various mechanisms:
- Re-traumatization: Substance abuse can lead to situations where individuals are more likely to experience further trauma, such as physical or sexual abuse, accidents, or involvement in violence, perpetuating a cycle of trauma and addiction.
- Re-traumatization in the context of trauma’s impact on addiction refers to the process by which individuals who have experienced past trauma are subjected to situations, environments, or stimuli that trigger the distressing memories and emotions associated with their original traumatic experiences. This phenomenon is particularly significant for individuals struggling with addiction, as it can exacerbate both their traumatic symptoms and substance use behaviors. Key aspects of re-traumatization in this context include:
- Triggering of Traumatic Memories: Exposure to certain cues or situations can trigger memories of past trauma. For someone with a history of trauma and addiction, these triggers can lead to increased substance use as a form of coping or escape.
- Heightened Emotional Responses: Re-traumatization can result in heightened emotional responses such as fear, anxiety, anger, or sadness. These intense emotions can drive an individual towards substance use to regulate or numb these feelings.
- Worsening of PTSD Symptoms: For those with PTSD, re-traumatization can worsen symptoms like flashbacks, nightmares, and hyperarousal. This intensification of symptoms can increase reliance on substances to manage these distressing experiences.
- Avoidance Behaviors: To avoid re-traumatization, individuals may engage in avoidance behaviors, which can include increased substance use to numb themselves from potential triggers or environments that remind them of the trauma.
- Impact on Recovery Efforts: Re-traumatization can pose significant challenges to recovery from addiction. It can lead to setbacks, relapses, and can make the treatment process more complex.
- Vulnerability in Treatment Settings: Certain aspects of addiction treatment, such as group discussions or confrontation about substance use, can inadvertently lead to re-traumatization if not handled with sensitivity to the individual’s trauma history.
- Difficulty in Establishing Trust: Re-traumatization can make it difficult for individuals to trust healthcare providers or support systems, which is crucial for effective treatment and recovery from addiction.
- Physical Health Consequences: Repeated activation of the stress response due to re-traumatization can have adverse effects on physical health, including exacerbating any existing health issues related to addiction.
- Social and Relational Impact: Re-traumatization can strain personal relationships and social interactions, as individuals may become withdrawn or exhibit behaviors that are difficult for others to understand or support.
- Need for Trauma-Informed Care: This underscores the importance of trauma-informed care in addiction treatment, where providers are aware of and sensitive to the trauma histories of their clients and can create a safe environment that reduces the risk of re-traumatization.
- Addressing re-traumatization is critical in the treatment of individuals with a history of trauma and addiction. It requires a comprehensive, empathetic approach that acknowledges and integrates the individual’s trauma experiences into their addiction treatment plan.
- Re-traumatization in the context of trauma’s impact on addiction refers to the process by which individuals who have experienced past trauma are subjected to situations, environments, or stimuli that trigger the distressing memories and emotions associated with their original traumatic experiences. This phenomenon is particularly significant for individuals struggling with addiction, as it can exacerbate both their traumatic symptoms and substance use behaviors. Key aspects of re-traumatization in this context include:
- Complicating Recovery: Trauma can complicate the recovery process from addiction. Traumatic memories and symptoms can trigger substance use as a coping mechanism, making it more challenging to achieve and maintain sobriety.
- Trauma significantly complicates the recovery process in individuals struggling with addiction. The interplay between trauma and addiction creates a complex set of challenges that can make recovery more difficult. Understanding these challenges is crucial for developing effective treatment strategies. Key aspects of how trauma complicates recovery from addiction include:
- Triggering of Trauma Symptoms: Recovery can often bring up unresolved trauma, leading to the re-emergence or intensification of trauma symptoms like flashbacks, nightmares, and severe anxiety. These symptoms can be overwhelming and may drive an individual back to substance use as a coping mechanism.
- Emotional Regulation Difficulties: Trauma often impairs the ability to regulate emotions. During recovery, as individuals no longer use substances to numb their feelings, they may find it difficult to cope with intense emotional responses, increasing the risk of relapse.
- Trust Issues and Relationship Challenges: Trauma can lead to difficulties in forming trusting relationships, including with therapists, counselors, and peer support groups. Trust and social support are critical components of effective addiction recovery.
- Increased Relapse Risk: The stress and emotional turmoil associated with trauma can increase the risk of relapse. Traumatic memories or triggers can lead to cravings and substance use as a form of self-medication.
- Dual Diagnosis Complexity: Many individuals with trauma and addiction have a dual diagnosis, meaning they struggle with both mental health disorders and substance use disorders. This complexity requires integrated treatment approaches that address both issues simultaneously.
- Avoidance Behaviors: Trauma survivors often develop avoidance behaviors to escape trauma-related thoughts and memories. During recovery, the absence of substances can make these memories and thoughts more pronounced, leading to a temptation to use substances again to avoid facing trauma.
- Challenges in Treatment Engagement: Trauma can make it challenging for individuals to engage fully in the treatment process. They may be more likely to miss sessions, find it hard to participate actively, or drop out of treatment programs.
- Physical Health Issues: Trauma and addiction can both have detrimental effects on physical health. The combined impact can complicate recovery, as individuals may need to manage physical health issues alongside addiction treatment.
- Compromised Coping Strategies: Trauma survivors often rely on substances as their primary coping strategy. Recovery requires the development of new, healthy coping mechanisms, which can be a challenging and lengthy process.
- Need for Specialized Treatment Approaches: Standard addiction treatment programs may not be sufficient for those with trauma histories. Specialized approaches, such as trauma-informed care and therapies specifically designed to address trauma, are often necessary.
- Safety and Stability Concerns: Creating a sense of safety and stability is crucial for individuals recovering from trauma and addiction. This can include safe housing, financial stability, and a supportive social environment.
- In summary, trauma complicates the recovery process from addiction by presenting additional psychological, emotional, social, and physical challenges. Effective treatment must be trauma-informed, addressing both the addiction and the underlying trauma, and providing a comprehensive, empathetic approach to support the individual through the complexities of their recovery journey.
- Trauma significantly complicates the recovery process in individuals struggling with addiction. The interplay between trauma and addiction creates a complex set of challenges that can make recovery more difficult. Understanding these challenges is crucial for developing effective treatment strategies. Key aspects of how trauma complicates recovery from addiction include:
- Co-Occurring Disorders: Trauma is often associated with mental health disorders like PTSD, anxiety, and depression. These co-occurring disorders can interact with addiction in complex ways, requiring integrated treatment approaches.
- Co-occurring disorders, also known as dual diagnosis, refer to the presence of both a mental health disorder and a substance use disorder in an individual. In the context of trauma’s impact on addiction, co-occurring disorders are particularly significant. The experience of trauma often leads to mental health issues that can coexist with, and even drive, substance abuse. Key aspects of co-occurring disorders in this context include:
- Post-Traumatic Stress Disorder (PTSD): One of the most common co-occurring disorders with addiction in individuals who have experienced trauma is PTSD. Symptoms of PTSD, such as flashbacks, nightmares, and hyperarousal, can lead individuals to self-medicate with drugs or alcohol.
- Depression and Anxiety: Trauma can result in depression and various forms of anxiety, which individuals may attempt to alleviate through substance use. This can create a cycle where the substance abuse exacerbates the mental health disorder, and vice versa.
- Complex Diagnosis and Treatment: The presence of co-occurring disorders complicates both diagnosis and treatment. Symptoms of mental health disorders and substance abuse can overlap, making it challenging to disentangle the two and address them effectively.
- Integrated Treatment Approach: Effective treatment for individuals with trauma-related addiction and co-occurring disorders requires an integrated approach that addresses both the substance use and the mental health disorder simultaneously.
- Increased Severity of Symptoms: Individuals with co-occurring disorders often experience more severe symptoms of both mental health issues and addiction, and may have a higher risk of suicide, compared to those with a single disorder.
- Reinforcement of Disorders: The relationship between trauma-induced mental health disorders and substance abuse can be mutually reinforcing. Substance abuse can worsen the symptoms of mental health disorders, while the distress from mental health issues can increase reliance on substances.
- Risk of Misdiagnosis: There’s a risk that one disorder may be overlooked or misdiagnosed, particularly if the symptoms of one are more prominent. This can lead to inadequate treatment and poor outcomes.
- Challenges in Engagement and Retention: Engaging and retaining individuals with co-occurring disorders in treatment can be more challenging. They might require more intensive and longer-duration treatment.
- Relapse Prevention: In individuals with trauma and co-occurring disorders, relapse prevention must address triggers related to both the mental health disorder and substance use.
- Need for Comprehensive Care: Treatment should include a range of services, including medical care, psychotherapy, medication management, and support for social and practical needs.
- Holistic Approaches: Addressing co-occurring disorders often requires holistic approaches that go beyond treating symptoms to include support for lifestyle changes, stress management, and the development of healthy coping mechanisms.
- In summary, the presence of co-occurring mental health disorders in individuals who have experienced trauma and are struggling with addiction adds complexity to both understanding and treating their conditions. An integrated, holistic approach that addresses the full spectrum of the individual’s needs is crucial for effective treatment and long-term recovery.
- Co-occurring disorders, also known as dual diagnosis, refer to the presence of both a mental health disorder and a substance use disorder in an individual. In the context of trauma’s impact on addiction, co-occurring disorders are particularly significant. The experience of trauma often leads to mental health issues that can coexist with, and even drive, substance abuse. Key aspects of co-occurring disorders in this context include:
- Emotional Regulation Difficulties: Trauma survivors often struggle with emotional regulation. Substances may be used as a way to manage overwhelming emotions or to fill emotional voids.
- Emotional regulation difficulties are a common and significant issue in the context of trauma’s impact on addiction. Trauma, especially when unaddressed or unresolved, can severely disrupt an individual’s ability to manage and process emotions effectively, leading to a reliance on substances as a coping mechanism. Key aspects of emotional regulation difficulties in this context include:
- Heightened Emotional Responses: Individuals who have experienced trauma may have heightened emotional responses. They might feel emotions more intensely or react more strongly to situations that others might find less distressing.
- Difficulty Identifying Emotions: Trauma can make it challenging to identify and understand one’s emotions. This lack of emotional awareness can lead to confusion and distress, with substances used as a means to numb or escape these feelings.
- Impaired Coping Mechanisms: Trauma often impairs healthy coping mechanisms. Individuals may turn to drugs or alcohol as a way to manage overwhelming emotions or to provide temporary relief from emotional pain.
- Dissociation and Numbing: In an effort to regulate intense emotional responses, individuals may dissociate or emotionally numb themselves. Substance use can be a tool for achieving this numbing effect, especially in cases of severe or chronic trauma.
- Reactivity and Impulsivity: Trauma can lead to increased impulsivity and reactivity. In moments of high stress or emotional overwhelm, individuals may impulsively use substances without considering the consequences.
- Mood Swings: Fluctuations in mood are common, with individuals experiencing rapid and intense shifts in emotions. These mood swings can be difficult to manage and may increase dependency on substances to stabilize mood.
- Anxiety and Panic Attacks: Experiences of trauma can trigger anxiety and panic attacks. Substances may be used in an attempt to control or alleviate these intense episodes of anxiety.
- Avoidance of Emotional Processing: Individuals may use substances to avoid confronting or processing traumatic memories and the associated emotions, hindering emotional healing and resolution of trauma.
- Increased Stress and Tension: Chronic stress and tension resulting from trauma can lead to a perpetual state of emotional dysregulation. Substances might be used to relieve this tension.
- Impact on Relationships: Difficulties in emotional regulation can strain personal and social relationships, as individuals may struggle to communicate effectively or react inappropriately in emotional situations.
- Triggering of Traumatic Memories: Emotional dysregulation can also trigger memories of the traumatic event, creating a cycle where substance use increases to manage the re-experiencing of trauma.
- Addressing emotional regulation difficulties is a crucial aspect of treatment for individuals with a history of trauma and addiction. This often involves therapeutic interventions aimed at developing healthier coping and emotional processing skills, alongside treatment for substance use disorders. Techniques like cognitive-behavioral therapy, dialectical behavior therapy, mindfulness practices, and trauma-informed approaches are often effective in improving emotional regulation.
- Emotional regulation difficulties are a common and significant issue in the context of trauma’s impact on addiction. Trauma, especially when unaddressed or unresolved, can severely disrupt an individual’s ability to manage and process emotions effectively, leading to a reliance on substances as a coping mechanism. Key aspects of emotional regulation difficulties in this context include:
- Impaired Social Functioning: Trauma can impair social and relational skills, leading to isolation and difficulties in forming healthy relationships. Substance use can be a way to alleviate feelings of loneliness or social anxiety.
- Impaired social functioning is a notable consequence in the context of trauma’s impact on addiction. Traumatic experiences, especially when unresolved, can significantly disrupt an individual’s ability to engage in and maintain healthy social interactions and relationships. This impairment can further complicate both the trauma and the addiction. Key aspects include:
- Withdrawal and Isolation: Trauma survivors often withdraw from social interactions and relationships. This can be due to feelings of shame, fear of judgment, or a desire to hide their substance use. Isolation can exacerbate feelings of loneliness and depression, potentially leading to increased substance use.
- Difficulty Trusting Others: Trauma, particularly relational trauma like abuse or betrayal, can lead to difficulties in trusting others. This distrust can hinder the formation of supportive relationships and can make it challenging to seek or accept help.
- Communication Challenges: Individuals with a history of trauma and addiction may struggle with effective communication. They might find it hard to express their needs, emotions, and experiences, which can lead to misunderstandings and conflicts in relationships.
- Altered Perception of Social Cues: Trauma can affect the ability to accurately read and respond to social cues. This can result in inappropriate or misinterpreted reactions in social settings, further impairing social interactions.
- Impaired Relationship Boundaries: Trauma can lead to difficulties in setting and maintaining healthy boundaries in relationships. Individuals might become overly dependent on others, or conversely, might push others away to avoid potential harm.
- Impact on Family Relationships: Trauma and addiction can strain family dynamics. Family members may not understand the individual’s behaviors or know how to support them effectively, leading to tension and conflict.
- Social Anxiety: Trauma can increase feelings of anxiety in social situations. This anxiety can be so overwhelming that individuals avoid social interactions altogether, or they might use substances to cope with or mask their anxiety.
- Engagement in Risky Behaviors: Impaired social functioning can lead to engagement in risky behaviors, including substance abuse in unsafe environments or forming relationships with individuals who encourage or enable substance use.
- Difficulty in Professional Settings: Trauma and addiction can impair professional relationships and performance. Challenges include difficulty concentrating, maintaining professional boundaries, and handling stress or criticism in the workplace.
- Re-traumatization in Social Contexts: Social situations can sometimes trigger memories of past trauma, leading to avoidance of social interactions and reliance on substances to cope with these triggers.
- Addressing impaired social functioning in the treatment of trauma and addiction involves a multifaceted approach. This includes therapy focused on building trust, communication skills, and healthy relationship patterns; support groups to foster a sense of community; family therapy to improve family dynamics; and developing coping strategies for managing social anxiety and avoiding risky behaviors. Encouraging the individual to gradually engage in safe social activities is also an important aspect of recovery.
- Impaired social functioning is a notable consequence in the context of trauma’s impact on addiction. Traumatic experiences, especially when unresolved, can significantly disrupt an individual’s ability to engage in and maintain healthy social interactions and relationships. This impairment can further complicate both the trauma and the addiction. Key aspects include:
- Impact on Treatment: Addressing trauma is an essential part of effective addiction treatment. Without treating the underlying trauma, the risk of relapse remains high.
- The impact of trauma on the treatment of addiction is profound and multi-dimensional. Trauma can significantly influence how individuals respond to addiction treatment, presenting unique challenges and considerations for effective care. Understanding and addressing these impacts is crucial for successful recovery. Key aspects include:
- Need for Trauma-Informed Care: Effective treatment for individuals with trauma-related addiction requires a trauma-informed approach. This means recognizing the presence of trauma and its impact, ensuring that treatment settings are safe and supportive, and using approaches that do not re-traumatize the individual.
- Integrated Treatment for Dual Diagnosis: Since trauma often coexists with addiction and other mental health disorders, integrated treatment that addresses both the trauma and the substance use disorder is essential for effective care.
- Building Trust and Safety: Individuals with trauma histories may have difficulties in trusting healthcare providers and may feel unsafe in treatment settings. Building a therapeutic relationship based on trust and safety is a crucial first step in treatment.
- Addressing Complex Emotional Needs: Treatment must address the complex emotional issues related to trauma, such as fear, shame, guilt, and anger, which can be barriers to recovery if left unaddressed.
- Challenges in Engagement and Retention: Individuals with trauma-related addiction may find it more difficult to engage with treatment and may be at higher risk of dropping out. Continuous support and encouragement are essential to maintain engagement.
- Risk of Re-traumatization: Care must be taken to avoid re-traumatization during treatment. This involves being sensitive to potential triggers and avoiding confrontational or aggressive therapeutic techniques.
- Tailoring Treatment Approaches: Treatment approaches should be tailored to the individual’s specific trauma history and symptoms. What works for one person may not be effective for another.
- Use of Specific Therapies: Therapies that are particularly effective for trauma, such as Eye Movement Desensitization and Reprocessing (EMDR), trauma-focused cognitive-behavioral therapy, and somatic experiencing, may be incorporated into the treatment plan.
- Impact on Group Therapy: Group therapy sessions, while beneficial, may need to be approached with caution. Sharing traumatic experiences in a group setting can be triggering for some individuals.
- Relapse Prevention: Trauma can increase the risk of relapse. Treatment should include comprehensive relapse prevention planning, with strategies to manage trauma-related triggers.
- Longer Duration of Treatment: Individuals with trauma-related addiction may require a longer duration of treatment to address the complexities of their situation adequately.
- Aftercare Planning: Post-treatment support is crucial. This includes continued therapy, support groups, and possibly ongoing medication management for co-occurring mental health conditions.
- In summary, the impact of trauma on addiction treatment necessitates a nuanced, patient-centered approach that acknowledges and integrates the individual’s trauma experiences into their addiction treatment plan. This comprehensive approach is essential for addressing the root causes of addiction and supporting long-term recovery.
- The impact of trauma on the treatment of addiction is profound and multi-dimensional. Trauma can significantly influence how individuals respond to addiction treatment, presenting unique challenges and considerations for effective care. Understanding and addressing these impacts is crucial for successful recovery. Key aspects include:
- Need for Trauma-Informed Care: Treatment for individuals with a history of trauma and addiction should be trauma-informed, meaning it recognizes the effects of trauma and integrates this understanding into all aspects of treatment and care.
- The need for trauma-informed care in the context of addiction treatment, especially when addressing the impacts of trauma, is crucial. Trauma-informed care is an approach that recognizes and responds to the effects of all types of trauma, emphasizing physical, psychological, and emotional safety for both providers and survivors. This approach helps survivors rebuild a sense of control and empowerment. Key aspects of the need for trauma-informed care include:
- Acknowledging the Prevalence of Trauma: Trauma-informed care starts with the understanding that trauma is prevalent among individuals with substance use disorders. This approach recognizes the role of trauma in the development and continuation of addiction.
- Creating a Safe Environment: A fundamental aspect of trauma-informed care is creating a treatment environment where individuals feel safe and supported, both physically and emotionally. This sense of safety is critical for individuals to open up and engage in treatment.
- Avoiding Re-traumatization: Trauma-informed care aims to avoid practices and interventions that may inadvertently re-traumatize individuals. This involves being mindful of potential triggers and the effects that various treatment approaches may have on those with trauma histories.
- Empowerment and Choice: Empowering individuals in their recovery process is a key tenet of trauma-informed care. This involves giving them choices and control over their treatment and recovery process, which helps in rebuilding a sense of autonomy and self-efficacy.
- Integrating Knowledge About Trauma: Treatment approaches are informed by knowledge about the impact of trauma on the brain, behavior, and relationships. This knowledge guides the development of effective strategies for addressing trauma and addiction.
- Holistic Approach: Trauma-informed care addresses the holistic needs of the individual, including physical, emotional, social, and spiritual well-being.
- Cultivating Resilience: This approach focuses on building resilience and identifying strengths, rather than solely addressing deficits or pathologies. It emphasizes recovery and the development of new coping skills.
- Cultural Competence: Trauma-informed care is culturally competent and sensitive to the individual’s background and identity, recognizing that different people process trauma in diverse ways.
- Collaborative Treatment Planning: Involving individuals actively in their treatment planning fosters a collaborative approach and ensures that care is tailored to their specific needs and trauma experiences.
- Staff Training and Support: Implementing trauma-informed care requires training for all staff members, not just clinical personnel, to ensure they understand trauma’s impact and how to interact with clients effectively and compassionately.
- Recognition of Signs and Symptoms: Staff are trained to recognize the signs and symptoms of trauma in clients and respond appropriately to their needs.
- Continuity of Care: Trauma-informed care often involves continuity of care post-treatment, recognizing that recovery is an ongoing process that requires ongoing support.
- Incorporating trauma-informed care into addiction treatment acknowledges the complex interplay between trauma and substance use and is essential for providing effective, compassionate, and holistic care to individuals on their recovery journey.
- The need for trauma-informed care in the context of addiction treatment, especially when addressing the impacts of trauma, is crucial. Trauma-informed care is an approach that recognizes and responds to the effects of all types of trauma, emphasizing physical, psychological, and emotional safety for both providers and survivors. This approach helps survivors rebuild a sense of control and empowerment. Key aspects of the need for trauma-informed care include:
- Holistic Approach: Successful treatment often requires a holistic approach that addresses not only the addiction but also the psychological, emotional, and social impacts of trauma.
- A holistic approach in the context of addressing the impact of trauma on addiction involves treating the whole person, not just the symptoms of addiction or the trauma. This approach recognizes that lasting recovery and wellness depend on addressing the interconnected aspects of an individual’s life, including physical, psychological, social, and spiritual dimensions. Key aspects of a holistic approach include:
- Physical Health: Addressing any physical health issues that may have arisen from addiction or trauma, such as chronic pain, sleep disturbances, or nutritional deficiencies. This also includes promoting physical wellness through exercise, proper nutrition, and adequate rest.
- Mental and Emotional Well-being: Providing therapies and interventions that address not only the addiction and trauma but also any co-occurring mental health disorders such as depression, anxiety, or PTSD. This includes therapies like cognitive-behavioral therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and other trauma-informed therapeutic modalities.
- Social Support: Fostering a supportive social environment is crucial. This involves strengthening existing healthy relationships, building new supportive networks, and possibly participating in group therapy or support groups like Narcotics Anonymous (NA) or other peer-support groups.
- Spiritual Care: Addressing spiritual needs, which can be an important aspect of healing for many individuals. This might involve practices like meditation, mindfulness, engagement in faith communities, or exploring personal beliefs and values.
- Lifestyle Changes: Encouraging and supporting lifestyle changes that promote overall health and well-being. This can include stress management techniques, engaging in hobbies and interests, and developing a balanced daily routine.
- Coping Skills Development: Teaching and reinforcing healthy coping mechanisms to deal with stress, triggers, and cravings. This is essential for managing both trauma-related symptoms and the challenges of recovery from addiction.
- Mind-Body Techniques: Incorporating mind-body techniques such as yoga, tai chi, or acupuncture can be beneficial. These practices can help in reducing stress, improving physical and mental balance, and enhancing overall well-being.
- Empowerment and Autonomy: A holistic approach empowers individuals in their recovery journey, giving them the tools and resources to take control of their health and make informed decisions about their treatment and lifestyle.
- Customized Treatment Plans: Recognizing that each individual’s experience with trauma and addiction is unique, holistic treatment plans are tailored to meet the specific needs of each person.
- Continuity of Care: Ongoing support and care are important components of a holistic approach. Recovery is viewed as a continuous journey, with the need for ongoing engagement in health-promoting activities and possibly continued therapy or support groups.
- By addressing all aspects of an individual’s life and well-being, a holistic approach to treating trauma’s impact on addiction can lead to more comprehensive and sustainable recovery outcomes. This approach not only helps individuals to overcome addiction and cope with trauma but also supports their overall quality of life and long-term health.
- A holistic approach in the context of addressing the impact of trauma on addiction involves treating the whole person, not just the symptoms of addiction or the trauma. This approach recognizes that lasting recovery and wellness depend on addressing the interconnected aspects of an individual’s life, including physical, psychological, social, and spiritual dimensions. Key aspects of a holistic approach include:
In summary, trauma can significantly influence the development, maintenance, and treatment of addiction. Recognizing and addressing the role of trauma is crucial in providing effective care for individuals struggling with substance use disorders.